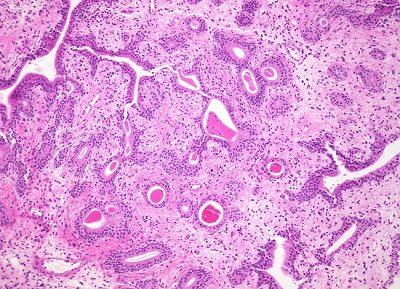
A change that occurs in the tissue that lines the bladder can be called cystitis glandularis. It is cystitis glandularis if a metaplastic transformation of mucosal cells lining the urinary bladder. Distinguishing the metaplastic change from urothelial cell carcinoma is the main importance in histopathology. It is a very common finding in bladder biopsies and cystectomies, and most often found in the trigone area. This particular type of tissue change is benign, but it can be a symptom of another health problem that needs to be treated. Non-mucinous and mucinous(intestinal) are two main types cystitis glandularis. In the metaplastic cells production of mucin, a normal feature of colonic and intestinal epithelial cells but not of urothelial cells, this is the difference.
Cystitis Glandularis Causes
A variety of patients who all have chronic bladder inflammation as uniting features have cystitis glandularis. The underlying causes include:
People who have chronic bladder irritation and inflammation
People who have a history of stones, bladder surgery, wear a catheter
Outlet obstruction of chronic bladder
Lipomatosis of pelvic
Prostatic hypertrophy which is benign
Bladder TCC
Infection of chronic
Calculi of bladder
Cystitis Glandularis Symptoms
Clinical Symptoms for Cystitis glandularis are as follows:
Recurrent frequency and urgency of urinating
Painful urination
Hematuresis
In lower abdomen and perineum, you can feel unusual pain
The opening of urethral orifice is painful and swelling
On the pubic area and perineum, you can feel unusual pain
Painful intercourse
Cystitis Glandularis Diagnosis
Cystoscopy: this method is a good way of cystitis glandularis diagnosis by inserting a camera into the bladder. The condition will be visible under magnification in a laboratory facility if a biopsy sample of tissue for the bladder is taken. Staining can help a laboratory technician learn more about the extent of the cellular changes and highlight the cell transformation.
CT: when one takes CT, hypervascular polypoid masses within urinary bladder can be seen.
MRI: when patient with condition to take the MRI, low signal polypoidal lesion, low signal lesion with central branching hyperintensity and central hyperintensity enhances on contrast administration, and represents vascular stalk can be observed.
Cystitis Glandularis Treatment
Treatments for the cause can include medications and surgery.
1. Medications
When treating cystitis glandular, some herbal medicines are also optional, such as Diuretic and Anti-inflammatory Pill, which can help one cure cystitis glandular safely and efficiently. It can kill bacteria and promote blood circulation and has no side effects.
2. Surgery
Treatment consists of removing the source of irritation and surgical excision of the area of inflammation or cystectomy in rare severe cases. An association with adenocarcinoma of the bladder has been described, and thus these patients should be monitored.
3. Tips after accepting treatment
A follow-up examination may be used to look for additional cellular changes once the patient has been treated. A patient with a history of this condition should make sure that it is noted in medical records so that other care providers will be aware of the issue. When making decisions about how best to diagnose and treat a urogenital health condition, it can become relevant. Because such patients are at increased risk of developing bladder malignancies, doctors may also recommend them be regularly screened for bladder cancer.
4. Building healthy eating habit and prevent cystitis glandular
Eat more diuretic food, such as water melon, grape, pineapple, celery, pear, etc.
Eat foods which can relieve the symptoms of urinary frequency and urgency as well as painful urination, such as escargots, corn, green soybean and scallion.
Drink water as much as possible and at least 1500ml of urine output every day should be kept.
Avoid spicy food like wine, pepper, vinegar, sour fruits, etc.
Avoid eating oranges because oranges may lead to alkaline urine that can accelerate the reproduction pace of bacteria.
Don’t drink much coffee because it can lead to the shrink of bladder neck and cause spasmodic pain.

